10,000 cases and counting
I noticed just before new year that a new patient I was assessing was the ten thousandth case since the clinic moved to a computerised notes system in 2010. I looked back to case 1 and low and behold case 10,000 and case number 1 were both back pain related to disc problems. This got me thinking about how back pain treatment has changed in this time or more importantly our knowledge of the mechanisms behind back pain. It also happens to be over 20 years since I qualified as a physiotherapist and without the benefit of access to all those cases I have treated in various countries around the world and numerous hours spent on the sides of pitches as a team physio or changing rooms I can’t be certain how many cases I’ve seen in those 20 years but it’s going to be somewhere in the region of double that.
I was told recently by a very experienced clinician that you don’t realise how much you know until you try to teach or train someone else. The things you take for granted that you think are so obvious have come from years and years of experience and fine tuning your radar and having seen it 10 thousand times before. So what have I learned about back pain in the last 20 years?
As a physiotherapy clinic we see a wide variety of musculoskeletal complaints from hip and knee pain, frozen shoulder, tennis elbow, pulled muscles and sprained ligaments but low back pain is still number one in terms of prevalence. This is unchanged in the last 20 years of practice however the reasons behind this have changed. 20 years ago people were having treatment for back pain because they were doing too much. For instance lifting things, digging things or falling off things. Now it’s because they are not doing enough. Life has become much more sedentary and as a consequence people have stiffened up, become weaker and get back pain when they try to do even the most basic manual stuff in the garden or start a new exercise regime. As mentioned in previous newsletters we can be very busy in our heads but not necessarily in our bodies so it is important to not confuse the two. Certainly over the last 20 years what people perceive to be an active lifestyle is very different to what it was in 1998.
As a result of this sedentary lifestyle people are starting to try and change their workstations by introducing Sit-Stand desks to break up the long periods of sitting. Unheard of in 1998 and starting to become a thing about 10 years ago and now in 2019 almost standard practice in new office buildings. There’s nothing new in standing up at work however. The chair dates back 5000 years but I’m told in the 16th century people stood to read at lecterns as it was considered vulgar to read sitting down and it was normal to stand in the 19th century working for official government bodies. In the 20th century we’d be familiar with the idea of an architect standing up working on their drawings. Hemmingway, Churchill and Da Vinci all worked in standing.

In the 1990’s MRI was seen as the answer to all back problems as the amazing detail of the spine was now visible in comparison to the basic images previously available with X-Ray. For the first time MRI showed us nerves and soft tissues and the holy grail – The Discs. The term slipped disc was coined due to the apparent appearance of these disc like structures having moved into the space where only nerves should be. Countless diagnosis of slipped disc were given and patients oblivious to the existence of these omnipotent rascals prior to MRI were convinced that the said discs would forevermore go flying out of their backs and out the window every time they bent over or sneezed from that moment on. Surgeons became very busy fusing spines to stop these things from moving or taking discs out and various forms of replacements put in to fill the gap to varying degrees of success.
20 plus years of research into MRI changes on normal spines has shown us that discs don’t move. They do change shape however and sometimes they hit nerves but the individual doesn’t necessarily experience pain when this happens. Some do, some don’t. The disc which was considered for a while to be the only reason someone would or wouldn’t have back pain is now considered normal if there is a bit of distortion to its shape especially in the lower vertebrae and as we get older. We have returned to putting more emphasis on the clinical findings and how well a back functions and less often MRI’s are being ordered as the changes reported on MRI which are not necessarily clinically relevant can lead to catastrophising by the patient which is unhelpful to the recovery process.
What MRI has really helped with is showing the quality of musculature especially the deepest layers of muscle, The Core and this has a significant role in a healthy spine and back pain. Surprisingly rarely reported on even now by Radiologists but I’ve no doubt we’ll see more reporting of the same in the years to come.

Over the last 20 years core muscles and core exercise have become buzz words in the exercise industry and still few people truly understand their significance. So with tens of thousands of consultations on back pain here is what it’s all about.
The core muscles control the segmental movement of the spine. That is they take care of what each individual vertebrae in the spine is doing so that the Global Muscles (these are the non-core muscles) can do the heavy work. The lifting, the pulling and the carrying. Basically the core looks after your spine so the rest of you can get on with things. So why would the core be a cause of back pain. Very simply if your core isn’t strong enough your back is inefficient. The discs and the joints take more strain and get wear and tear which becomes painful and the global muscles have to do two jobs. They have to hold you and move you at the same time which is inefficient and leads to fatigue and ultimately failure. This might be mechanical back pain or sciatica or potentially a disc prolapse that does compress nerves and generates a whole world of pain.
But do core exercises actually work. Well yes and no. Just because you do a core exercise, lets say The Plank, doesn’t actually mean you are using your core muscles. The segments that these core muscles work on need to be mobile enough to respond to core exercise and vice versa. So if your back is stiff or immobile in certain areas then all the core exercises in the world won’t develop your core at these levels.
Also, just because you can touch your toes doesn’t mean your spine is mobile. You might be HYPERmobile in some ares and HYPOmobile in others but eventually those HYPOmobile segments get weaker and can be the source of pain. As physios we spend most of our time identifying these stiff segments and getting them moving so that you as the patient can then respond to exercise to get stronger, efficient and pain-free.
If I think about the one thing that has changed most significantly since graduating from university and the 20 years of experience since has taught me, it is my understanding of pain and how it works and with back pain in particular. This has completely turned on it’s head what we thought back in the 1990’s.
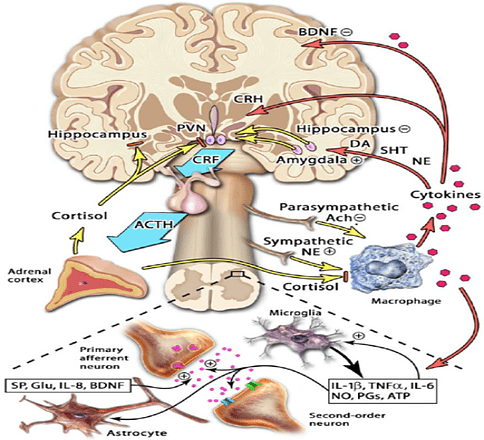
Is pain all in the brain. Yes, and it is fascinating. The pain gate theory by Melzack & Wall was our best understanding of pain back in the old days which put very simply gave us the idea that nerve fibres were stimulated in the injured part and through a process of gates some of these messages were allowed into the brain and some messages came back down and that’s how we experienced pain.
Now we understand it’s far more complex than that and our whole life journey plays a role in the pain experience we have. What back pain means to a person can be much more or less significant at any moment in time. For example your back “going” on the day of a big interview or presentation could be far more distressing than your back “going” on holidays and therefore the pain experience you have will be different. Getting back pain when someone close to you has a chronic back condition means you are more likely to think that’s how you’ll end up and therefore the pain experience will be different to for instance a professional wrestler who sees it as part of the job and pays it little attention.
What we do know is that all these receptors in your spine sending messages up through the spinal cord to the brain get processed by the limbic system – the emotional centres of the brain – and all our past experiences, belief systems and evidence available to us get analysed and sent to the motor cortex which is the part of the brain representing every part of the body and then we have a pain experience. That experience works both ways. If we believe we are going to get pain from something then we probably will.
Bed rest was common practice for treating back problems. Now you’re advised against it in all but extreme cases. We have to prove to the brain that things still work in order for the pain experience to be calibrated properly and recover from back pain.
Functional MRI scans where we can see what parts of the brain are responsible for certain things have helped us understand this process so perhaps MRI’s for back pain will include the brain in years to come and not just the spine itself so we can see how individuals interpret the pain experience and then effectively re-organise that from the top down as well as the bottom up.

So in summary after 20 years of doing this back pain is quite simple but complex at the same time. Most episodes of back pain are short lived and do not cause long term harm and do not need to become a recurring pattern.
All back pain has a mechanical component as well as a pain experience unique to the individual who’s back it is, however there are common drivers for interpretation and manifestation of that pain experience. Having seen this tens of thousands of times over the years patterns of behaviour and understanding emerge. There is a lot of mythology out there about back pain that persists which is not helpful for the individual with back pain and this can significantly impact on their pain experience and ultimately recovery. For example the term Slipped Disc has people believing that discs are slippery, wobbly things ready to pop out at any moment. If you believe that you’ll be terrified to bend over to tie your laces when your back hurts and that will make you stiffer, weaker and ultimately more painful.
The messages coming from our body go to the brain which houses all the information we have of past experiences and information we believe to be true, some of it helpful, some of it not so and then we get a pain response. From a physio point of view we need to get your spine mobile in order to get it stronger so that the messages going up to the brain in the first place are ones of improved movement and that changes the pain response.
MRI scans have their place but if it doesn’t influence management, it is not indicated. Clinical signs and the response to treatment are most important. Lifestyles have changed enormously in the last 20 years and we are generally more sedentary which isn’t great for our bodies. You might run or go to the gym but that’s maybe 3-4 hours a week and what are you like for the remaining 164 hours. Long periods of inactivity are no good for us and we need to be generally more active. A sit-stand desk can help but there’s nothing new in that and it’s not enough.
There is a lot of bad information out there and Dr. Google doesn’t necessarily have the right answers for you. It’s easy to make symptoms fit and then head down the wrong wormhole with a little knowledge, which is a dangerous thing. Such information will sit in the limbic system and ad in some shape or form to our pain experience in the future so be careful where you get your information from.
Be more mobile, get more mobile and get some expert advice. We’ve been at this a while and know a thing or two about back pain.




0 Comments